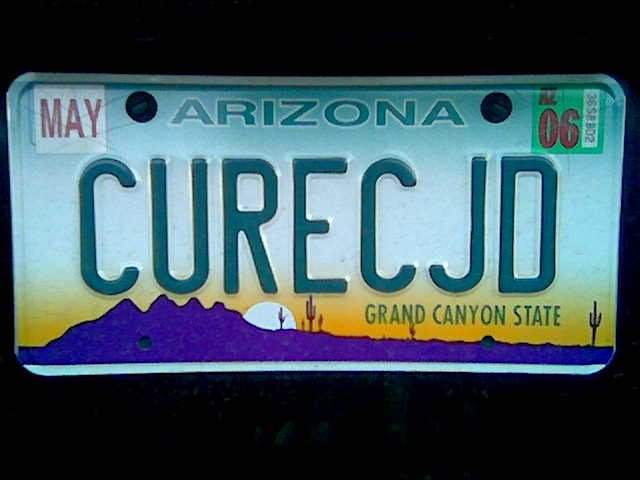
I just learned of a suspected-CJD patient who was thrown in a psych ward for her own safety. This is an outrage and absolutely deplorable at best. The doctors who made this decision should be ashamed of themselves.
Patient care is one of the most important aspects of CJD. Most doctors are not very informed at all, especially if you end up putting your relative in a smaller hospital. This is the typical arc of what goes wrong:
A patient begins to experience all manner of symptoms from forgetfulness to vertigo. There is usually blurry eyesight, gait problems, balance problems and myoclonus (jerky muscle movements). These were the symptoms my mother had by the time my father took her to the E.R. She was also combative by this time and experienced fits of anger.
At this point, the patient gets taken to the nearest hospital, as in a smaller hospital. A multitude of tests are run to no avail and doctors shake their heads mystified because it isn’t early-onset Alzheimer’s Disease, it isn’t Parkinson’s Disease, and it isn’t multiple sclerosis. There is still no diagnostic test that can be done to prove a patient has CJD; there is no clinical diagnosis. CJD is only proven upon final autopsy.
So as a patient is in the hospital with said symptoms, imagine the following scenario. It happens each time with differing degrees of drama and stress depending on the individual variables such as symptoms and length of disease.
A very frustrated family is angry with doctors and nurses who can’t explain why their loved one is rapidly deteriorating and losing all their faculties. I went through this myself, watching my mother lose a different ability almost each day. It was shocking. One day, she didn’t understand when she had to use the bathroom anymore, holding her urine for over 12 hours. A few days after her incontinence began, she lost the ability to swallow and had to be fed through a tube.
At this point, an even more stressed and frustrated family manages to transfer their loved one to a larger hospital, a teaching hospital maybe, or at least something more equipped to handle this ‘mystery’ disease. More tests are endured, less results are delivered because CJD is so hard to diagnose, and the patient and family are both suffering horribly. Patients are not receiving drugs necessary to make them more comfortable, or they are still receiving useless physical therapy, or worse; getting thrown in a psych ward.
Here is where I am outraged. My mother was lucky enough to be under the care of Dr. Russell Walker at Barrow Neurological Institute. I have heard horror stories from others who weren’t so lucky. Nurses were unafraid to touch my mother, but I have heard of some other families who have had to deal with this fear. I have heard of families banging their heads against the wall trying to get proper medication for a loved one who is combative and hallucinating. Since CJD patients often cannot communicate as they lose the ability to speak and experience aphasia, they cannot ask for meds. They cannot tell you if/when they are in pain. They cannot tell you what is wrong and they cannot ask for help.
I always felt a severe disconnect with my mother as she was dying because she could not speak to me. We couldn’t tell what she wanted, what she saw when she hallucinated, we couldn’t understand any words that came out of her mouth; it was awful. I am sure she knew she was dying, but she didn’t know what was killing her. We weren’t able to say goodbye to her and she couldn’t say goodbye to us. It’s a bad enough situation as it is. Families have to go on FMLA and hopefully they can afford to not work for months. Many families are already caring for elderly relatives when CJD strikes, as was my mother’s case. She was a healthy, 55-year-old woman who took care of a mother with Alzheimer’s and a father with numerous health problems.
We need to make the situation easier for CJD families everywhere, and that begins with better education of doctors at all hospitals, not just the big ones. Many of us are involved in this year’s CDC-sponsored CJD Medical Education Project facilitated by the CJD Foundation. We are hitting all the big hospitals and I will be going to Barrow Neurological to see Dr. Walker and her colleagues later this year. Hopefully next year, we can go into smaller hospitals and educate the doctors and nurses who are usually the first to encounter a case of CJD. Think of them as first responders.
It does not make it easier when a family is mistreated by an uneducated hospital. I have recently learned of a family with a 55-year-old mother who has a suspected case of CJD with the most severe onset of symptoms I’ve heard of in a while. She is having severe hallucinations, is combative and is angry. The hospital in question told the family she needed to be put in a psych ward for her own safety after she fell and broke a wrist.
There is no excuse for this. A CJD patient, or suspected CJD patient should never be placed in a psych ward. I feel from my own personal experience that a patient can be properly medicated and cared for at any hospital of any size without having to be demeaned by being thrown into a pysch ward. If a patient has CJD, they aren’t going to benefit from a psych ward at all. They have no control of themselves and never will again. Caretakers must concentrate their energies on making the end of life as peaceful and comfortable as possible.
My mother responded well to seizure meds when she got to BNI. I am not sure what specific drugs she was given to calm her down, but I’m hoping some other CJD families will comment on that. I have been meaning to obtain my mother’s records from BNI to find out what worked for her so I can tell other families, but life happens. The nurses at BNI were fantastic, even padding her bed because of her seizures and myoclonus. That’s all you need to do; treat the patient with respect, give the proper meds to keep the patient calm and provide some padding in the bed. My mom may have had to be tied down at one point in bed, but I can’t remember. She did have to be tied to a chair when sitting up and also had to be propped up with pillows. We all worked very hard to keep her as comfortable as possible. A psych ward never entered the equation. CJD patients need to be in the neuro ward, not the psych ward.
I can say this was frightening news as someone who has a family history of CJD. As we carry the E200K gene in my family, I have a 50% chance of developing this disease. I have yet to be tested. I am not sure if I will get tested but I do know if I am to die as my mother did that I most certainly would never want to end up mistreated in a psych ward.